In 1996, after six months of seeking a diagnosis for a strange set of symptoms that didn’t seem to fit I was diagnosed as having myelofibrosis, a rare, life threatening bone marrow disease for which there is no cure apart from a very high risk bone marrow transplant.
Myelofibrosis is essentially caused by a problem in the messaging system of the bone marrow in which the collagen within the marrow, instead of being flexible and acting like oil in a machine, becomes increasingly fibrous as scar tissue forms. Eventually the scar tissue fills the marrow cavity and the marrow can no longer produce blood. Until then the blood that is produced is poor quality, as shown by abnormal blood counts and incorrectly shaped blood cells.
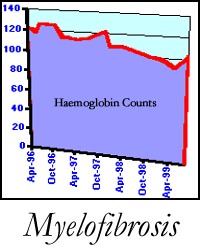
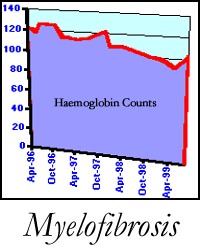
In my case I have steadily declining red blood cells and platelets, while my white counts are way too high. The low red counts mean that I have severe anaemia and am easily tired. The low platelets eventually pose a threat of uncontrollable bleeding, as platelets are essential for clotting. The poor quality blood affects all other organs as blood is the source of nourishment and takes away waste within the body’s system.
The skin is particularly affected, as is the digestive system. As well, unusual activity within the marrow can cause pain within the bones, which is difficult to control through medication.
Myelofibrosis can arise on its own or can occur after a previous blood disorder (usually many years later). It is most commonly found at the end of a person’s life when it is one of a number of health problems leading to death. It is not common in younger people such as myself and it is thought that there are probably fewer than 25 people in Australia who have primary myelofibrosis who are not old people. I know of one child.
The cause is not known but it seems likely that there needs to be a combination of factors for it to occur:
One very common associated problem is that the spleen attempts to manufacture blood to supplement the marrow and this effort causes it to enlarge. An enlarged spleen can cause a lot of discomfort as it presses on other organs in the abdomen and is painful when touched. Also, the liver becomes affected, as it too attempts to produce blood.
In my case as I look back to try to determine when this disease could have begun I notice that I had abnormal liver counts when I had an Executive Health Check about 8 years ago. But the check did not include a CBC (complete blood count) and I was told to stop drinking so much. As I did not drink more than two glasses of wine a week I found this hard to understand and ignored it. Confirmation of diagnosis requires a bone marrow biopsy, a difficult process of extracting marrow from inside the pelvic bones. Often the marrow will be so fibrous that it is difficult to extract a sample. This is in itself an indication of the disease and its progress. (After a terrible experience with gas as the anaesthetic I now request strong sedation and pain relief before this procedure.)
As the disease progresses, weight loss occurs and the person develops a body with a large stomach but thin elsewhere. Night sweats are also common also easy bleeding and bruising, not only on the limbs but also gums become rather delicate. I have had periods where I had a lot of small bleeds under the skin and unexplained bruises on my legs. I am very careful with my feet, for example when gardening, as injuries take a long time to heal.
Most people find the fatigue the single most difficult symptom. I have had times where I cannot climb one flight of stairs without puffing and panting and pausing part way up.
But you can learn to manage the symptoms and get on with your life on a curtailed basis.
For those who see illness as a metaphor for emotional problems, myelofibrosis presents an interesting challenge. It is like a slow strangling of the life force from within, like concrete cancer in a high rise building, that can’t be seen until it is too late to do anything to stop it.
It is extremely difficult to determine how long you can live with myelofibrosis until you have a pattern of blood counts over a period of time from which you can see a pattern of decline occurring. I have heard of people having a long slow decline over 12 – 15 years. On the other hand some people have an aggressive form which sees their death in less than a year. I was diagnosed aged 48 and told I had years rather than decades left to live, and judging by my blood counts subsequently that prediction will be accurate unless I undertake my only chance of a cure, a bone marrow transplant.
For more detailed information about myelofibrosis and access to the Internet chat group of which I am an active member go to:
http://inform.acor.org/mpd/mffaq.html[Main]
All content ©1999-2005 Sharyn Cederman
Designed by Tim Cederman-Haysom. To contact me email me at tim at cederman com